Gut Health: A comprehensive guide to treating the cause
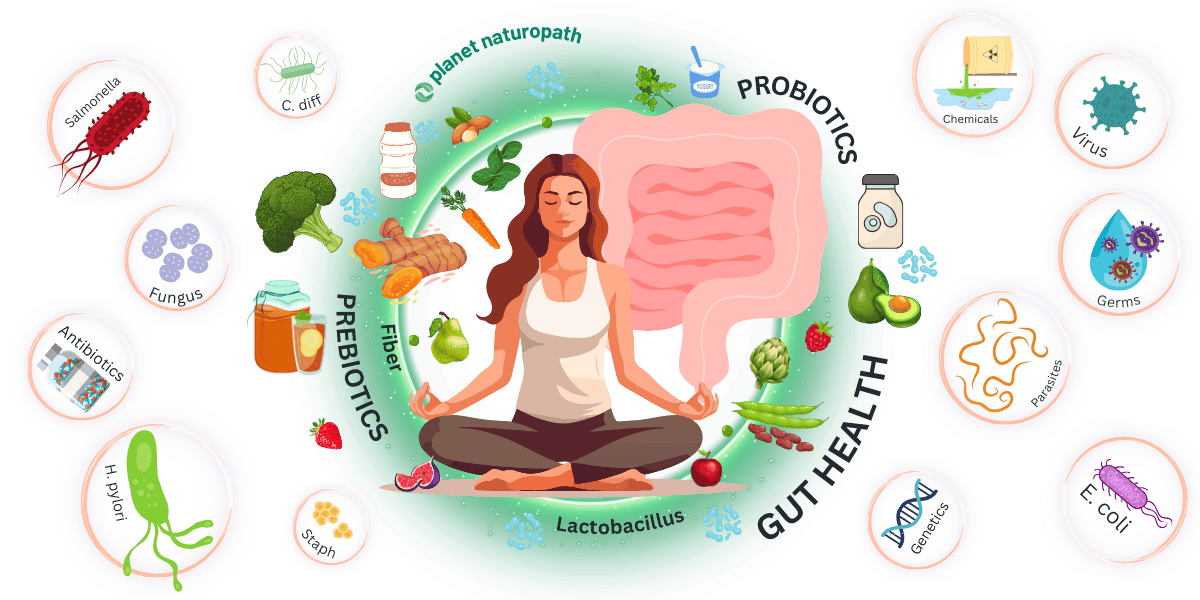
Gut health is one of the keys to your overall well-being, affecting everything from digestion and nutrient absorption to immune function and mental health.
Unlike traditional approaches that focus on alleviating symptoms, at Planet Naturopath we focus on identifying the root causes of digestive issues to provide lasting solutions.
The gut is home to trillions of microorganisms, collectively known as the gut microbiome, which play a vital role in maintaining health.
A balanced gut microbiome supports proper digestion, synthesizes essential nutrients, and protects against harmful pathogens.
However, when this balance is disrupted, it can lead to a range of digestive problems and systemic health issues.
Table Of Contents
- Why Choose a Functional Medicine Approach to Gut Health?
- Understanding Reflux (GERD)
- Helicobacter Pylori Infection
- Gallbladder Disease and Preventing Gallstones
- Do You Need Digestive Enzymes?
- Are You Experiencing Gut Bloating?
- SIBO – The Number One Cause of IBS
- Do You Have Leaky Gut?
- Treating Irritable Bowel Syndrome (IBS)
- Managing Inflammatory Bowel Disease (IBD)
- Celiac Disease and Gluten Intolerance
- Food Intolerances and Sensitivities
- The Low FODMAP Diet for IBS
- Prebiotics and Probiotics For Optimal Gut Health
Why Choose a Functional Medicine Approach to Gut Health?
While traditional medicine focuses on treating symptoms when they occur with medications or even surgery, we focus on identifying and addressing the underlying causes of gut health issues.
Through advanced diagnostic testing, including stool tests like Gut Zoomer and GI Map, and SIBO breath tests, we gain a comprehensive understanding of your gut health.
This allows us to create personalized treatment plans that go beyond symptom relief, promoting long-term health and vitality.
Our Comprehensive Testing Methods
Our practice is distinguished by our use of detailed testing methods to uncover the specific imbalances and issues in your digestive system.
These tests provide invaluable insights into the state of your gut health, guiding us in crafting targeted, effective treatment strategies.
By understanding the root causes, we can address issues such as bacterial overgrowth, infections, and food sensitivities with precision.
What to Expect from This Guide
In this comprehensive guide to gut health, we’ll explore the various aspects of maintaining a healthy gut, common digestive issues, and the steps you can take to improve your gut health naturally.
We’ll also link to more detailed articles on specific topics, providing a wealth of information to support your journey to optimal health.
|
Condition |
Test |
|---|---|
|
Reflux (GERD) | |
|
Helicobacter Pylori Infection | |
|
Gallbladder Disease | |
|
Digestive Enzymes | |
|
Gut Bloating | |
|
Small Intestinal Bacterial Overgrowth (SIBO) | |
|
Leaky Gut | |
|
Irritable Bowel Syndrome (IBS) | |
|
Inflammatory Bowel Disease (IBD) | |
|
Celiac Disease | |
|
Food Intolerances and Sensitivities |
Understanding Reflux (GERD)
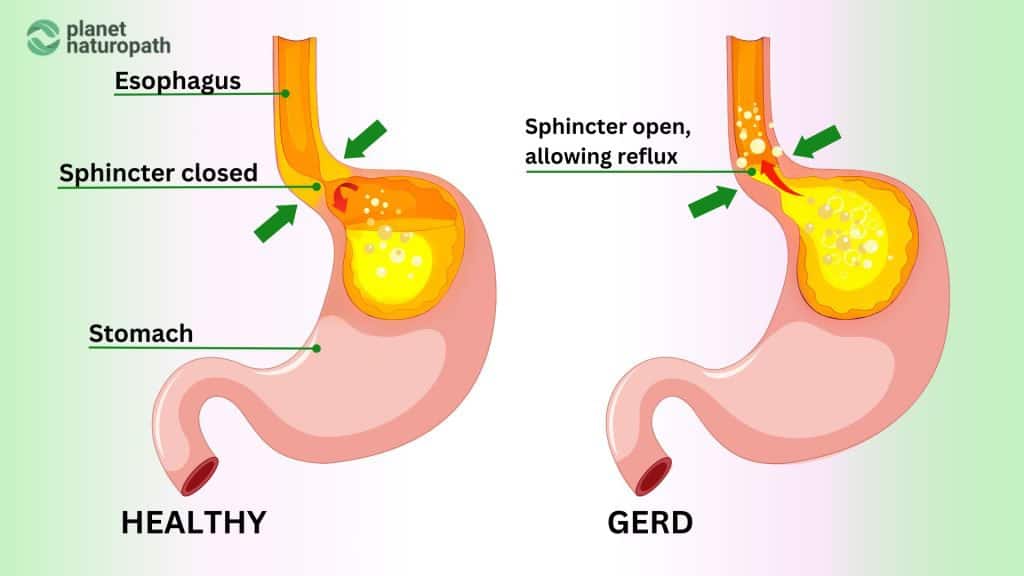
What is Reflux?
Gastro-esophageal reflux disorder, commonly known as GERD, acid reflux, reflux, or simply heartburn, is a prevalent condition affecting millions of people globally. While the clinical term is GERD, we’ll refer to it as reflux or heartburn for simplicity.
Reflux occurs when stomach acid travels up into the esophagus, causing a burning sensation in the chest and sometimes the throat. This is why it’s often called heartburn, despite having no relation to the heart.
Another form, known as “silent reflux,” doesn’t cause the typical burning sensation but leads to a buildup of mucus in the throat, resulting in a chronic dry cough or frequent need to clear the throat.
Common Symptoms of Reflux
Reflux can manifest in various symptoms, including:
- Burning Sensation: A burning feeling in the chest or throat.
- Regurgitation: A sour or bitter-tasting acid backing up into the throat or mouth.
- Bloating and Belching: Feeling bloated or frequent belching.
- Nausea: Feeling sick to the stomach.
- Chronic Cough: Especially with silent reflux, leading to a persistent dry cough.
- Throat Issues: Hoarseness, sore throat, or a frequent need to clear the throat.
Note: You don’t need to have all of these symptoms and sometimes people only have 1 or 2.
Causes of Reflux
Several factors can contribute to the development of reflux, including:
- Dietary Choices: Foods that are spicy, fatty, or acidic can trigger reflux. Common culprits include chocolate, caffeine, gluten, alcohol, and citrus fruits.
- Lifestyle Factors: Obesity, smoking, and lying down soon after eating can increase the risk of reflux.
- Medical Conditions: Conditions like hiatal hernia can lead to reflux.
- Medications: Some medications can relax the lower esophageal sphincter, leading to reflux.
Why Treating the GERD Symptoms Isn’t Enough
Many people rely on over-the-counter medications like Mylanta or prescription proton pump inhibitors (PPIs) such as Pariet, Losec, or Nexium to alleviate the symptoms of reflux.
While these medications can be effective in managing symptoms, they do not address the underlying causes of the condition.
In fact, long-term use of PPIs can lead to dependency and may worsen symptoms once the medication is stopped.
Furthermore, untreated or poorly managed reflux can result in serious health problems, such as ulceration, esophageal cancer, hormone imbalances, and nutrient malabsorption.
Related Post
Helicobacter Pylori Infection
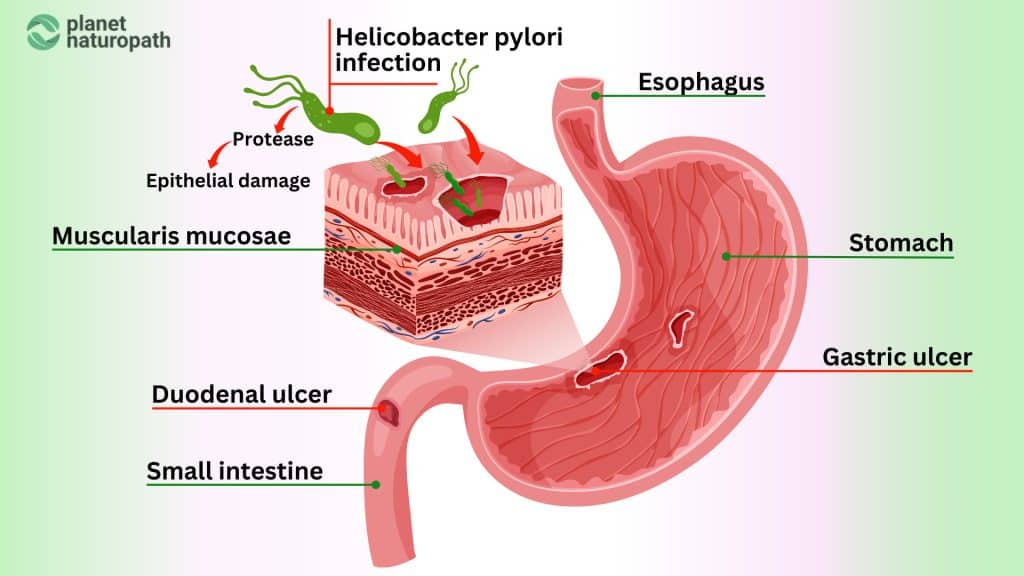
What is Helicobacter Pylori Infection?
Helicobacter pylori (H. pylori) is a type of bacteria that infects the stomach lining, leading to chronic inflammation and a variety of gastrointestinal issues.
This infection is quite common, affecting about half of the world’s population, although many people may not exhibit symptoms, if symptoms are not present then treatment may not be necessary.
Common Symptoms of H. Pylori Infection
While some individuals with H. pylori infection remain asymptomatic, others may experience a range of symptoms, including:
- Abdominal Pain: A burning or gnawing pain in the stomach, which can be more pronounced on an empty stomach.
- Bloating: A feeling of fullness or bloating after eating small amounts of food.
- Nausea and Vomiting: Persistent nausea and occasional vomiting.
- Loss of Appetite: Reduced desire to eat, which can lead to unintentional weight loss.
- Frequent Burping: Excessive belching, particularly after meals.
- Indigestion: A general discomfort or unease in the upper abdomen.
- Fatigue: Feeling unusually tired or lethargic.
In more severe cases, H. pylori infection can lead to:
- Peptic Ulcers: Open sores that develop on the lining of the stomach or the upper part of the small intestine.
- Gastrointestinal Bleeding: Blood in vomit or stool, which can indicate a bleeding ulcer.
- Increased Risk of Stomach Cancer: Chronic infection and inflammation can increase the risk of developing gastric cancer.
Causes of H. Pylori Infection
H. pylori infection is primarily spread through:
Poor Hygiene Practices: Lack of proper sanitation and hygiene can facilitate the spread of H. pylori.
Contaminated Food and Water: Consuming food or water that is contaminated with the bacteria.
Person-to-Person Contact: Close contact with an infected person, such as through saliva, can spread the bacteria.
Testing H. Pylori Infection
At Planet Naturopath we use the GI Map test as the main test for H.pylori as it also assesses the virulence factors, this helps to understand if the infection is serious and warrants treatment even if a person may not have symptoms.
Another good test for H.pylori is the Vibrant Wellness Gut Zoomer test

Vibrant Wellness Gut Zoomer Test
Related Post
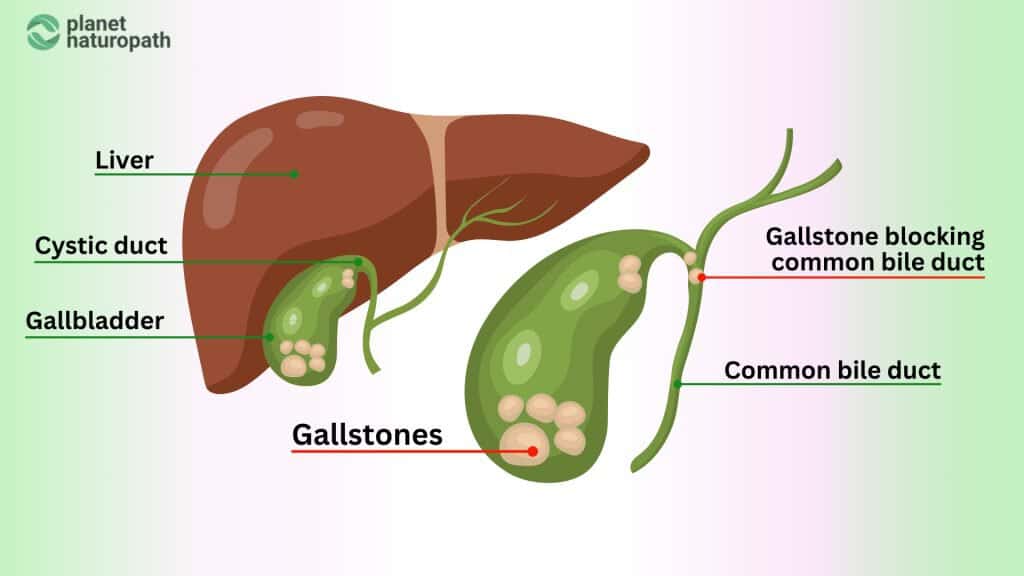
Gallbladder Disease and Preventing Gallstones
What is Gallbladder Disease?
Gallbladder disease encompasses various conditions that affect the gallbladder, a small organ located beneath the liver.
Its primary function is to store and concentrate bile, a digestive fluid produced by the liver.
One of the most common issues related to the gallbladder is gallstones, which are hardened deposits of digestive fluid that can form in the gallbladder.
Gallstones can range in size from tiny grains to large stones and can cause significant pain and digestive problems.
Common Symptoms of Gallbladder Disease
Gallbladder disease can present a variety of symptoms, particularly when gallstones block the bile ducts. Common symptoms include:
- Abdominal Pain: Severe, sudden pain in the upper right abdomen, which may radiate to the back or right shoulder. This pain often occurs after eating fatty or greasy foods.
- Nausea and Vomiting: Persistent nausea and vomiting, especially after meals.
- Indigestion: Bloating, heartburn, and gas.
- Jaundice: Yellowing of the skin and eyes, which indicates a blockage in the bile ducts.
- Fever and Chills: Often a sign of gallbladder infection (cholecystitis).
Causes of Gallstones
Several factors can contribute to the formation of gallstones, including:
- Excess Cholesterol in Bile: When the liver excretes too much cholesterol, it can crystallize and form stones.
- Excess Bilirubin in Bile: Conditions that cause excessive breakdown of red blood cells can lead to higher levels of bilirubin, which can contribute to gallstone formation.
- Incomplete Emptying of the Gallbladder: If the gallbladder doesn’t empty properly or often enough, bile can become overly concentrated, leading to stone formation.
Risk Factors for Gallbladder Disease
Certain factors increase the risk of developing gallstones, such as:
- Obesity: Excess body weight increases the amount of cholesterol in bile.
- Diet: High-fat, high-cholesterol, and low-fiber diets can increase the risk.
- Age and Gender: Gallstones are more common in women and older adults.
- Family History: A family history of gallstones can increase the risk.
- Certain Medical Conditions: Conditions like diabetes, liver disease, and certain blood disorders.
Why It’s Important to Address Gallbladder Disease
Untreated gallstones can lead to severe complications, including inflammation, infection, and even rupture of the gallbladder.
Chronic gallbladder disease can significantly impact digestion and overall quality of life. In some cases, surgical removal of the gallbladder (cholecystectomy) may be necessary to resolve persistent issues.
Related Post
Do You Need Digestive Enzymes?
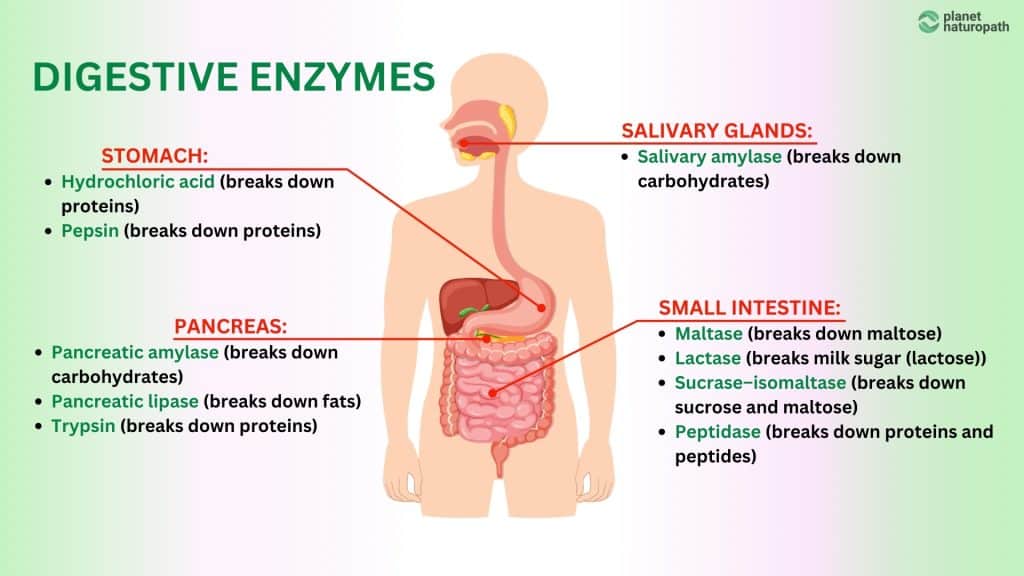
What are Digestive Enzymes?
Digestive enzymes are specialized proteins produced by the body to help break down the food we eat into absorbable nutrients.
These enzymes play a crucial role in the digestive process, ensuring that proteins, fats, and carbohydrates are broken down into their simplest forms so that they can be absorbed into the bloodstream and utilized by the body.
The primary sources of digestive enzymes include the salivary glands, stomach, pancreas, and small intestine.
Common Symptoms of Enzyme Deficiency
When the body doesn’t produce enough digestive enzymes, it can lead to a range of digestive issues, including:
- Bloating and Gas: Excess gas and bloating after meals.
- Abdominal Pain: Discomfort or pain in the abdomen after eating.
- Diarrhea or Constipation: Irregular bowel movements.
- Undigested Food in Stool: Visible undigested food particles in the stool.
- Nutrient Deficiencies: Signs of malnutrition despite a balanced diet.
Do You Really Need Digestive Enzymes?
The necessity of digestive enzyme supplements varies from person to person. While the body typically produces sufficient enzymes, certain conditions and lifestyle factors can impair enzyme production.
Here’s a closer look at who might benefit from supplemental digestive enzymes:
Who Might Need Digestive Enzymes:
- Individuals with Pancreatic Insufficiency: Conditions like chronic pancreatitis, cystic fibrosis, and pancreatic cancer can reduce enzyme production.
- Aging Adults: Enzyme production can decrease with age, leading to digestive issues.
- People with Specific Health Conditions: Conditions like lactose intolerance, IBS, and certain autoimmune diseases can benefit from enzyme supplementation.
- Those with Poor Diets or Overeating: Diets high in processed foods and overeating can overwhelm the digestive system, necessitating extra enzyme support.
Who Might Not Need Digestive Enzymes:
- Healthy Individuals with Balanced Diets: Most people with a healthy, balanced diet do not need enzyme supplements.
- Temporary Digestive Issues: Occasional digestive discomfort usually doesn’t require long-term enzyme supplementation.
The Role of Digestive Enzymes in Digestion
The process of breaking down food into absorbable nutrients begins in the mouth, where enzymes in saliva start breaking down carbohydrates.
This continues in the stomach with the help of stomach acid and pepsin, which primarily break down proteins.
The most significant enzyme activity occurs in the small intestine, where the pancreas releases a mix of digestive enzymes, including:
- Proteases: Break down proteins into amino acids.
- Lipase: Breaks down fats into fatty acids and glycerol.
- Amylase: Breaks down carbohydrates into simple sugars like glucose and fructose.
These enzymes ensure that the food we eat is effectively broken down into nutrients that the body can absorb and use.
Why Addressing Digestive Health Matters
Effective digestion is crucial for overall health, as it ensures the body receives the necessary nutrients to function correctly.
While digestive enzyme supplements can be beneficial for those with specific deficiencies or conditions, it’s essential to identify and address the root causes of digestive issues.
Over-reliance on supplements without addressing underlying problems can lead to ongoing health challenges.
Related Post
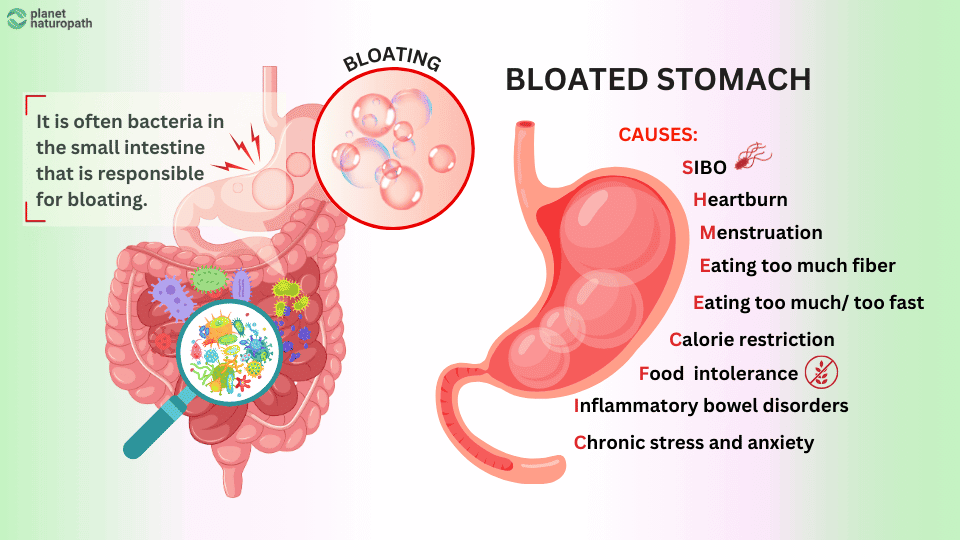
Are You Experiencing Gut Bloating?
What is Bloating?
Bloating is one of the most common and annoying digestive symptoms that I see in the clinic, it involves a feeling of fullness, tightness, or swelling in the abdomen.
This uncomfortable sensation often occurs after eating and can be accompanied by visible distension of the abdomen.
Bloating can range from mildly annoying to severely uncomfortable and is usually fine in the morning and gets worse throughout the day.
Common Symptoms of Bloating
Bloating can present with a variety of symptoms, including:
- Abdominal Fullness: A sensation of being overly full or tight in the abdomen.
- Visible Swelling: Noticeable distention or swelling of the stomach area.
- Excessive Gas: Increased belching or flatulence.
- Pain and Discomfort: Abdominal pain or cramps.
- Rumbling or Gurgling: Noises from the digestive tract as it processes food and gas.
Causes of Bloating
Several factors can contribute to bloating, including dietary habits, lifestyle choices, and underlying health conditions:
Dietary Causes
- High-Fiber Foods: Consuming large amounts of fiber-rich foods like beans, lentils, and certain vegetables can produce excess gas.
- Carbonated Drinks: Drinking sodas and other carbonated beverages introduces gas into the digestive system.
- Dairy and Gluten Products: Lactose intolerance can cause bloating when consuming dairy products. Gluten is a common trigger for bloating.
- High-FODMAP Foods: Certain carbohydrates (FODMAPs) found in foods like onions, garlic, and wheat can be difficult to digest for some people.
Lifestyle Causes
- Eating Too Quickly: Swallowing air while eating too quickly can contribute to bloating.
- Overeating: Eating large meals can stretch the stomach and cause bloating.
- Lack of Exercise: Physical inactivity can slow down digestion and increase bloating.
- Stress: High stress levels can affect digestive enzymes and motility
Health Conditions
- Irritable Bowel Syndrome (IBS): A common condition that can cause bloating, along with other digestive symptoms. IBS is often caused by SIBO.
- Small Intestinal Bacterial Overgrowth (SIBO): An overgrowth of bacteria in the small intestine can lead to bloating. This is probably the most common cause of bloating.
- Gastroparesis: Delayed stomach emptying can cause bloating and discomfort.
How to Manage and Prevent Bloating
Managing and preventing bloating often involves dietary and lifestyle changes:
Dietary Adjustments
- Avoid Carbonated Drinks: Replace sodas with still water or herbal teas.
- Lactose-Free Options: Choose lactose-free dairy products if you are lactose intolerant.
- Low-FODMAP Diet: Identify and avoid high-FODMAP foods that trigger bloating.
Lifestyle Changes
- Eat Slowly: Take your time when eating to reduce the amount of air swallowed.
- Smaller Meals: Eat smaller, more frequent meals instead of large ones.
- Regular Exercise: Incorporate physical activity into your routine to help stimulate digestion.
Medical Interventions
- Probiotics: These can help balance gut bacteria and reduce bloating, but be careful if you have SIBO they have the potential to make things worse.
- Digestive Enzymes: Supplementing with enzymes can aid in the breakdown of difficult-to-digest foods.
- Further Testing: Testing helps to take out the guesswork with treatment plans, testing for SIBO with a breath test, and doing an advanced stool test like the Gut Zoomer to assess enzyme levels and other potential triggers like H.pylori
Related Post
SIBO – The Number One Cause of IBS
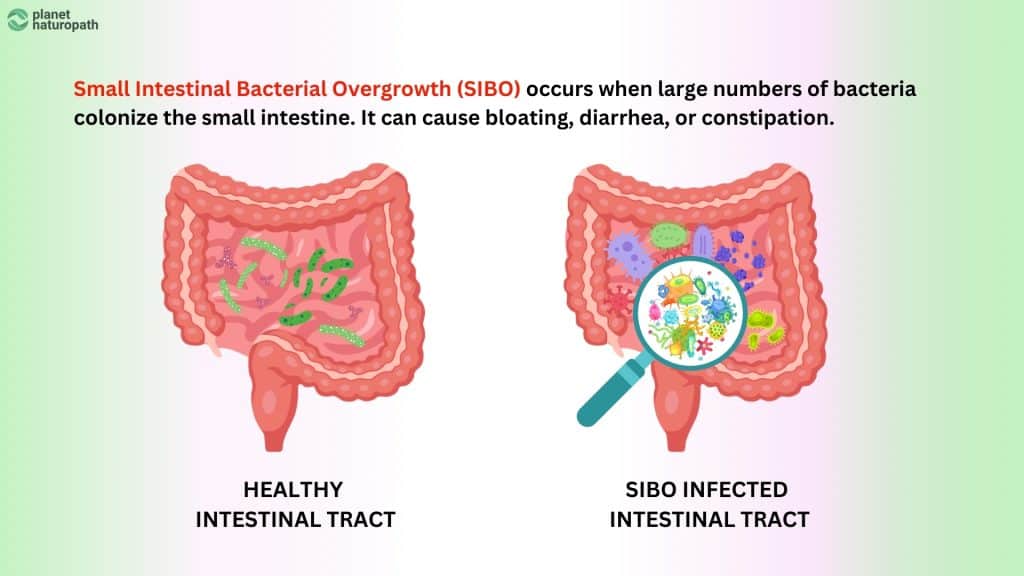
What is SIBO?
SIBO stands for Small Intestinal Bacterial Overgrowth. It’s a condition where excessive bacteria, normally found in the large intestine, proliferate in the small intestine.
Although awareness of SIBO is increasing among healthcare professionals, it remains underdiagnosed because it’s not widely covered in traditional medical education.
Much of the research on SIBO has emerged over the past decade, and many doctors may not be up-to-date with the latest findings.
As a result, individuals with SIBO-related symptoms are just told they have IBS and there is nothing that they can do about it.
Common Symptoms of SIBO
SIBO manifests through a range of digestive symptoms, many of which overlap with those of IBS. Common symptoms include:
- Bloating: A feeling of fullness and swelling in the abdomen.
- Abdominal Pain: Discomfort or cramping in the stomach area.
- Diarrhea: Frequent, loose, or watery stools.
- Constipation: Difficulty passing stools or infrequent bowel movements.
- Reflux: A burning sensation in the chest or throat caused by stomach acid rising up the esophagus.
- Gas: Excessive belching or flatulence.
Causes of SIBO
Several factors can contribute to the development of SIBO, including:
- Structural Abnormalities: Issues like intestinal strictures or adhesions can disrupt normal gut motility.
- Motility Disorders: Conditions that affect gut motility, such as diabetes or scleroderma, can lead to bacterial overgrowth.
- Medications: Long-term use of certain medications, such as proton pump inhibitors (PPIs), can alter gut flora and promote bacterial overgrowth. Antibiotics are another trigger for SIBO
- Food poisoning: Along with antibiotics food poisoning is one of the most common triggers of SIBO, people will usually quickly get over the initial food poisoning but then don’t feel right and continue to experience digestive symptoms.
How to Diagnose SIBO
Accurately diagnosing SIBO is essential for effective treatment. While standard diagnostic tests can rule out serious conditions like gastritis, polyps, or cancer, they cannot identify SIBO.
Specialized tests, such as breath tests measuring hydrogen and methane levels, are necessary to diagnose SIBO.
I recommend the Food Marble test, this is a device that you purchase and can use for multiple different tests which is often needed when diagnosing and also retesting for SIBO.
Contact us for more information about Food Marble as you need to be connected to a practitioner to get the full benefits of this device which includes the SIBO reports.
Managing SIBO
Treatment for SIBO typically involves a combination of dietary changes, herbal antimicrobials, and probiotics. Key strategies include:
- Dietary Modifications: Low-FODMAP diets can reduce the fermentation substrate for bacteria.
- Herbal Medicine: Specific herbs can target and reduce bacterial overgrowth.
- Probiotics and Prebiotics: These can help restore a healthy balance of gut flora.
- Motility Agents: Medications or supplements that enhance gut motility can help prevent recurrence.
Related Post
Don’t know where to start?
Schedule a consultation to review your current results or find out the next best test for you to do!
Do You Have Leaky Gut?
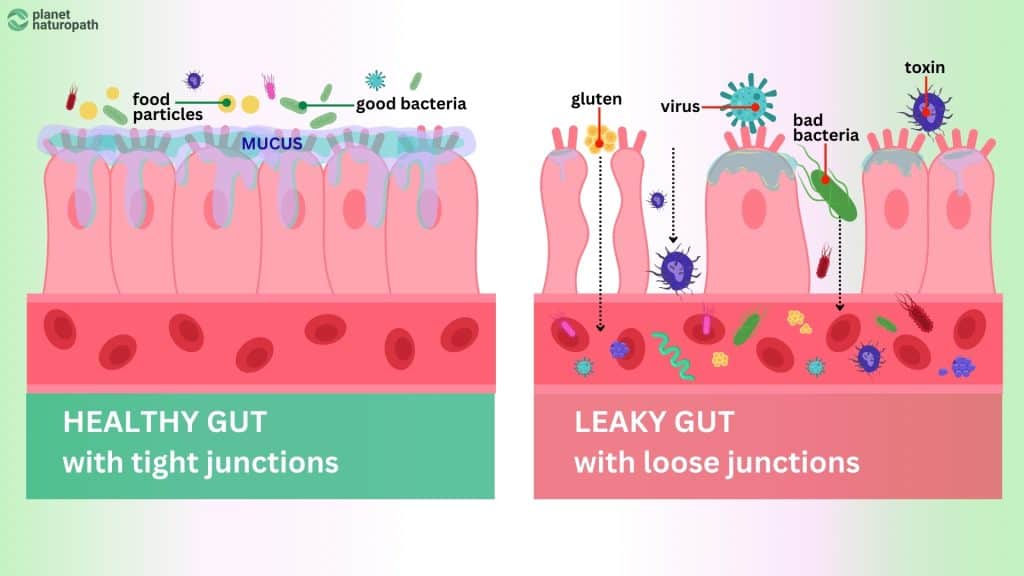
What is Leaky Gut?
Leaky gut, also known medically as intestinal permeability, is a condition where the lining of the small intestine becomes damaged, causing undigested food particles, toxins, and bacteria to leak into the bloodstream.
This leakage can trigger inflammation and provoke an immune response, leading to a variety of health issues both in the gut and also systemic symptoms.
Common Symptoms of Leaky Gut
Leaky gut can manifest through a wide range of symptoms, including:
- Digestive Issues: Bloating, gas, diarrhea, and constipation.
- Food Sensitivities: Increased sensitivity to certain foods, causing reactions like bloating, headaches, or rashes.
- Fatigue: Persistent tiredness and lack of energy.
- Joint Pain: Unexplained aches and pains in the joints.
- Skin Problems: Conditions like eczema, acne, or rosacea.
- Mood Disorders: Anxiety, depression, and other mood swings.
- Autoimmune Conditions: Worsening symptoms of autoimmune diseases like Hashimoto’s thyroiditis or rheumatoid arthritis.
Causes of Leaky Gut
Several factors can contribute to the development of leaky gut, including:
- Imbalanced Gut Microbiome: A lack of beneficial bacteria can compromise the integrity of the gut lining.
- Poor Diet: Diets high in refined sugars, processed foods, and alcohol can damage the gut lining.
- Chronic Stress: Persistent stress can weaken the gut barrier and increase intestinal permeability.
- Medications: Long-term use of NSAIDs, antibiotics, and other medications can disrupt the gut lining.
- Infections: Bacterial, viral, or fungal infections can damage the intestinal lining.
Testing for Leaky Gut

Vibrant Wellness Wheat Zoomer
This advanced test evaluates your immune response to gluten and wheat, as well as tests for intestinal permeability. It can identify specific antibodies like Zonulin that indicate damage to the gut lining, plus it can measure the levels of lipopolysaccharides which is an endotoxin from gut bacteria, this testing helps to diagnose leaky gut accurately.

Vibrant Wellness Gut Zoomer Test
The Gut Zoomer stool test also measures things like zonulin for leaky gut but this test is beneficial for identifying the potential causes of leaky gut, this can be high levels of LPS producing bacteria, parasites and candida.
Advanced Stool Testing
Identifying Triggers
Advanced stool tests, such as the GI Map, can help identify underlying triggers of leaky gut, such as bacterial imbalances, parasites, and yeast overgrowth.
These tests provide a comprehensive analysis of the gut microbiome, inflammation markers, and digestive function.
Advantages
By pinpointing specific imbalances and infections, advanced stool testing allows for targeted treatment plans to restore gut health and reduce intestinal permeability.
Managing Leaky Gut
Effective management of leaky gut involves a combination of dietary changes, supplements, and lifestyle adjustments
Dietary Modifications
Adopt an anti-inflammatory diet that includes whole foods, reduces processed foods, and eliminates known food sensitivities. Prebiotic foods are also helpful to increase your butyrate levels naturally.
Supplements
Probiotics, prebiotics, and specific nutrients like L-glutamine, butyrate, zinc carnosine, and omega-3 fatty acids can help repair and support the gut lining.
Stress Management
Techniques like meditation, yoga, and regular exercise can reduce stress and support gut health. The Nerva program is a gut-brain self-hypnosis program for IBS.
Avoiding Triggers
Identifying and eliminating foods or substances like alcohol and medications that trigger symptoms is crucial in managing leaky gut.
Leaky gut, or intestinal permeability, can have far-reaching effects on overall health.
Accurate testing through tools like the Vibrant Wellness Wheat Zoomer and advanced stool tests can provide valuable insights into the condition, allowing for personalized treatment plans.
By addressing the root causes and implementing targeted strategies, you can significantly improve gut health and overall well-being.
Related Post
Treating Irritable Bowel Syndrome (IBS)
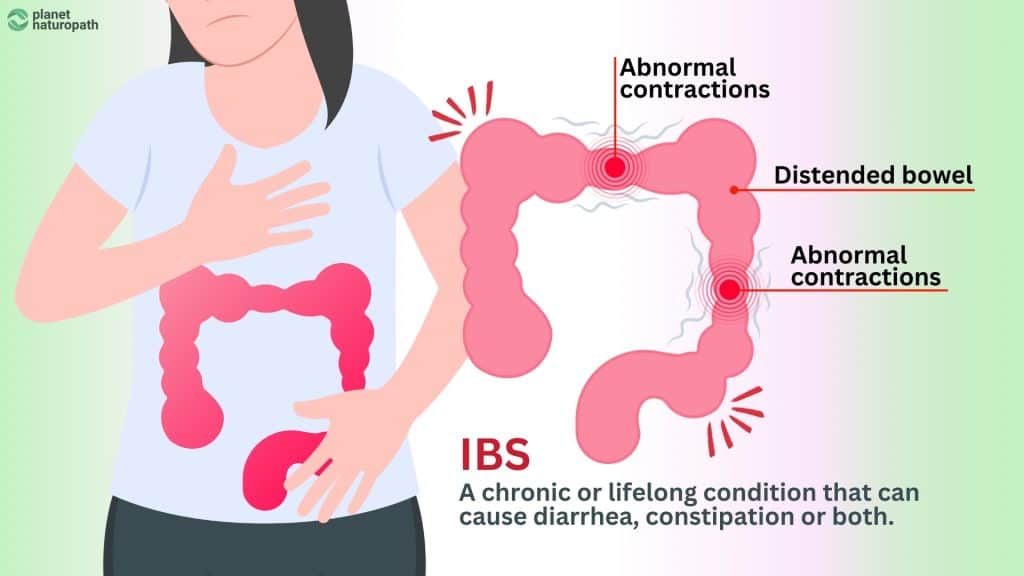
What is IBS?
Irritable Bowel Syndrome (IBS) is a common functional gastrointestinal disorder that affects the large intestine.
Unlike conditions with clear structural abnormalities, IBS is characterized by a group of symptoms that occur together, including chronic abdominal pain and altered bowel habits.
Despite its prevalence, IBS can be challenging to diagnose and manage, as the exact cause is not well understood and it often overlaps with other digestive disorders.
Often people are labeled with IBS but other conditions like SIBO, dysbiosis and pancreatic insufficiency have not been ruled out.
Common Symptoms of IBS
IBS symptoms can vary widely among individuals but typically include:
- Abdominal Pain and Cramping: Chronic pain or discomfort in the abdomen, often relieved by bowel movements.
- Altered Bowel Habits: This can include diarrhea (IBS-D), constipation (IBS-C), or a combination of both (IBS-M).
- Bloating and Gas: Excessive gas and a feeling of fullness or swelling in the abdomen.
- Mucus in Stool: Presence of white mucus in the stool.
- Urgency: A sudden, uncontrollable urge to have a bowel movement.
Causes and Triggers of IBS
While the exact cause of IBS is not known, several factors are thought to contribute to its development:
Food Sensitivities: Certain foods, especially those high in FODMAPs, dairy and gluten can trigger or worsen symptoms.
Gut-Brain Interaction: Abnormal communication between the brain and the gut can lead to altered motility and sensitivity.
Gut Motility Issues: Problems with how food moves through the digestive tract can cause diarrhea or constipation.
Infections: A history of severe gastrointestinal infection can increase the risk of developing IBS.
Gut Microbiome Imbalance: Dysbiosis, or an imbalance in the gut bacteria, can contribute to IBS symptoms.
Diagnosing IBS
Diagnosing IBS typically involves a combination of clinical evaluation and exclusion of other conditions. There is no specific test for IBS, but a healthcare provider may use the following methods:
- Symptom Review: Detailed assessment of symptoms based on established criteria (Rome IV criteria).
- Exclusion of Other Conditions: Tests to rule out other disorders, such as inflammatory bowel disease (IBD), celiac disease, and infections using advanced stool tests.
- Breath Tests: Tests for lactose intolerance or small intestinal bacterial overgrowth (SIBO) which can mimic IBS symptoms.
Managing IBS
Management of IBS often requires a personalized approach tailored to individual symptoms and triggers:
Dietary Changes
Implementing a low-FODMAP diet can significantly reduce symptoms for many people. Identifying and avoiding trigger foods is crucial.
However the low FODMAP diet is not a long term solution and should not be needed once the underling cause is addressed.
Stress Management
Techniques such as mindfulness, meditation, and cognitive-behavioral therapy (CBT) can help manage the stress and anxiety that often accompany IBS.
Herbal carminatives
Herbs like peppermint, ginger and fennel can help as well as Ayurvedic formulas like Triphala
Probiotics and Prebiotics
Certain probiotics can help balance gut bacteria and improve symptoms. Prebiotics can also be great to encourage the right bacteria and improve motility but often you have to start with low dosages.
Regular Exercise
Physical activity can help improve bowel function and reduce stress.
Importance of a Personalized Approach
Since IBS can present differently in each individual, a personalized treatment plan is essential. Doing advanced stool tests like the Gut Zoomer or GI Map test can be beneficial.
Testing for SIBO using a SIBO breath test or the Food Marble device can be helpful when deciding the best way to treat your digestive symptoms.
Related Post
Managing Inflammatory Bowel Disease (IBD)
What is IBD?
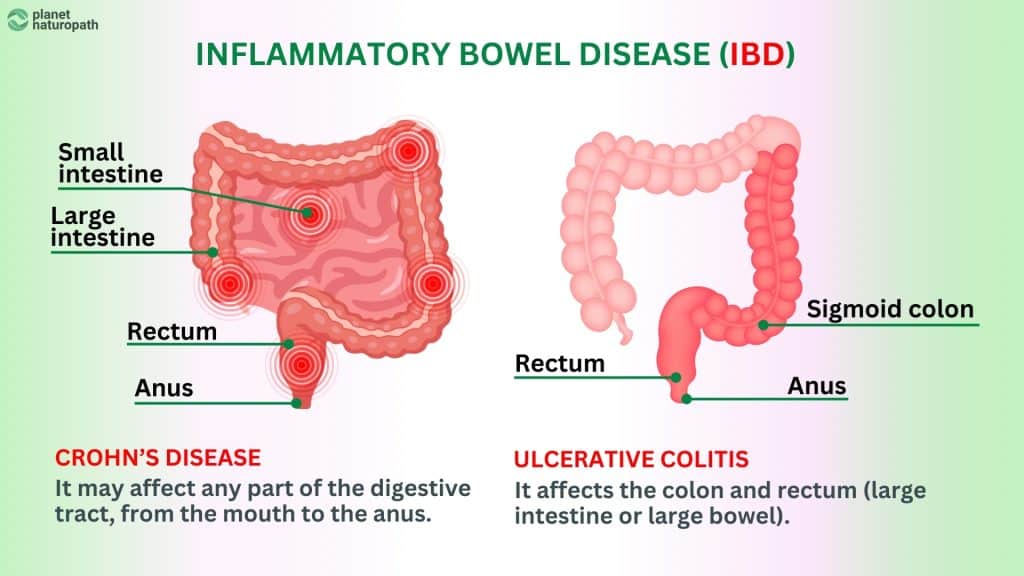
Inflammatory Bowel Disease (IBD) is a term used to describe chronic inflammatory conditions of the gastrointestinal tract, primarily Crohn’s disease and ulcerative colitis.
Unlike Irritable Bowel Syndrome (IBS), which affects the function of the gut, IBD involves actual structural damage to the digestive tract, leading to more severe symptoms and complications.
IBD requires medical management and ongoing monitoring to control inflammation and prevent flare-ups.
Common Symptoms of IBD
The symptoms of IBD can vary depending on the severity and location of the inflammation but typically include:
- Abdominal Pain and Cramping: Severe and persistent pain, often in the lower abdomen.
- Chronic Diarrhea: Frequent, loose, or watery stools, sometimes with blood or mucus.
- Fatigue: Persistent tiredness and lack of energy.
- Weight Loss: Unintentional loss of weight due to malabsorption and loss of appetite.
- Fever: Periodic fevers, particularly during flare-ups.
- Rectal Bleeding: Presence of blood in the stool, more common in ulcerative colitis.
- Urgency and Tenesmus: A constant urge to have a bowel movement and feeling of incomplete evacuation.
Causes and Triggers of IBD
The exact cause of IBD is not known, but it is believed to result from a combination of genetic, environmental, and immune system factors:
Microbiome Imbalance: Disruptions in the gut microbiome can contribute to inflammation. In particular low levels of Akkermnansia and Faecalbacterium prausnitzi are associated with IBD and can be assessed in advanced stool tests.
Genetic Predisposition: Family history of IBD increases the risk and you can assess your genetic risk through the SelfDecode gene test.
Immune System Dysregulation: Abnormal immune responses that attack the gut lining.
Environmental Factors: Factors such as diet, smoking, and infections can trigger or exacerbate IBD.
Diagnosing IBD
Diagnosis of IBD involves a comprehensive evaluation, including:
- Clinical Evaluation: Detailed medical history and symptom assessment.
- Endoscopy: Colonoscopy or sigmoidoscopy to visualize the gut and obtain biopsies.
- Imaging Studies: MRI, CT scans, or ultrasound to assess the extent and severity of inflammation.
- Laboratory Tests: Blood tests to check for anemia, inflammation markers, and stool tests for calprotectin levels to monitor inflammation and dysbiosis.
Managing IBD
Management of IBD typically involves a combination of medical treatments, dietary changes, and lifestyle modifications:
Medical Management
- Medications: Anti-inflammatory drugs (such as aminosalicylates), immunosuppressants, biologics, and corticosteroids are commonly used to reduce inflammation and control symptoms.
- Surgery: In severe cases, surgery may be necessary to remove damaged portions of the intestine or to treat complications.
Diet and Nutrition
- Anti-Inflammatory Diet: Incorporating anti-inflammatory foods and avoiding triggers like processed foods, dairy, and high-sugar foods.
- Nutrient-Dense Foods: Emphasizing a diet rich in vitamins, minerals, and proteins to address nutrient deficiencies and support healing.
- Hydration: Ensuring adequate fluid intake to prevent dehydration from chronic diarrhea.
Natural Approaches
- Probiotics and Prebiotics: Supporting a healthy gut microbiome can help manage symptoms.
- Supplements: Certain herbs like turmeric and aloe vera may help reduce inflammation, and nutrients like Butyrate and Glutamine can be helpful for gut healing. Quality supplements can make a big difference to your symptoms, for IBD I recommend Moss Nutrition.
- Stress Management: Techniques such as yoga, meditation, and the Nerva program can help manage stress, which can exacerbate IBD symptoms.
Advanced Testing
- Stool Tests: Comprehensive stool tests can identify gut microbiome imbalances, infections, and inflammation markers like calprotectin, which help monitor disease activity and guide treatment.
- Nutritional Assessments: Testing for nutrient deficiencies to tailor dietary and supplement recommendations.
Importance of Ongoing Monitoring and Personalized Care
Managing IBD requires regular monitoring to assess disease activity and adjust treatment plans as needed.
Advanced stool tests and periodic checks of calprotectin levels are crucial for tracking inflammation and preventing flare-ups.
At Planet Naturopath we can help support you during the treatment and maintenance of IBD.
Related Post
Celiac Disease and Gluten Intolerance
What is Celiac Disease?
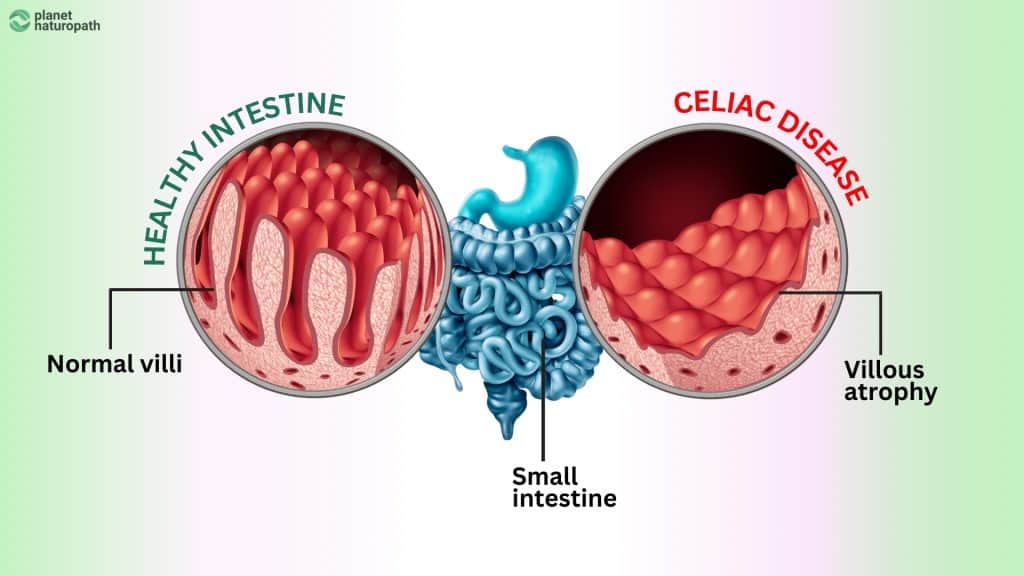
Celiac disease is an autoimmune disorder where the ingestion of gluten—a protein found in wheat, barley, and rye—triggers an immune response that damages the small intestine.
This damage impairs nutrient absorption and can lead to a wide range of health issues.
Unlike a simple food allergy, celiac disease involves an immune reaction that causes long-term harm to the gut lining and total avoidance of gluten is essential.
What is Gluten Intolerance?
Gluten intolerance, also known as non-celiac gluten sensitivity, is a condition where individuals experience symptoms similar to celiac disease but without the autoimmune response and intestinal damage.
While not as serious as celiac disease, gluten intolerance can cause digestive and other symptoms after consuming gluten that can be affect the quality of life and avoidance of gluten is recommended.
Common Symptoms of Celiac Disease and Gluten Intolerance
Both conditions share several symptoms, although celiac disease can cause more severe long-term health issues due to intestinal damage. Common symptoms include:
Digestive Issues: Bloating, gas, diarrhea, constipation, and abdominal pain.
Nutrient Deficiencies: Due to impaired nutrient absorption, symptoms can include anemia, fatigue, and weight loss. This mainly affects celiac disease.
Skin Issues: Dermatitis herpetiformis, an itchy skin rash, is specific to celiac disease but gluten intolerance can also contribute to skin conditions like eczema.
Neurological Symptoms: Headaches, brain fog, and neuropathy.
Joint Pain: Unexplained joint pain or inflammation.
Fatigue: Persistent tiredness and lack of energy.
Diagnosing Celiac Disease and Gluten Intolerance
Conventional Blood Testing for Celiac Disease
Standard blood tests for celiac disease, such as tTG-IgA and EMA tests, detect antibodies that indicate an autoimmune response to gluten.
While they can be effective for diagnosing celiac disease they are not 100% accurate, these tests do not identify non-celiac gluten sensitivity, leaving many individuals undiagnosed and untreated.
Vibrant Wellness Wheat Zoomer Test
The Wheat Zoomer test provides a detailed analysis of the immune response to various components of wheat and gluten.
It screens for antibodies associated with celiac disease, gluten sensitivity, wheat allergy, and intestinal permeability (leaky gut).
Unlike conventional tests, the Wheat Zoomer can detect both celiac disease and non-celiac gluten sensitivity.
It also helps identify early signs of intestinal damage and gut permeability, offering a more comprehensive understanding of how gluten affects an individual’s health.
Managing Celiac Disease and Gluten Intolerance
Management of both conditions primarily involves strict adherence to a gluten-free diet, but there are additional steps to support gut health and overall well-being:
Dietary Changes
- Gluten-Free Diet: Eliminating all sources of gluten from the diet is crucial. This includes avoiding foods containing wheat, barley, and rye.
- Cross-Contamination: Being vigilant about cross-contamination in food preparation and dining out to avoid accidental gluten ingestion.
- Nutrient-Rich Foods: Emphasizing whole, nutrient-dense foods to address and prevent nutrient deficiencies caused by malabsorption.
Supplements and Support
- Nutrient Supplements: Taking supplements to address deficiencies, such as iron, calcium, vitamin D, and B vitamins.
- Digestive Enzymes: Using gluten-specific enzymes to help break down trace amounts of gluten that may be accidentally ingested, these are not a green light to go ahead and deliberately eat gluten.
Ongoing Monitoring
- Regular Testing: Periodic testing with tools like the Wheat Zoomer can help monitor gluten sensitivity and gut health.
- Medical Follow-Up: Regular pathology testing is important to assess nutritional deficiencies which can help to guide supplementation.
Understanding the differences between celiac disease and gluten intolerance is essential for effective management, if you have celiac disease it is important that you avoid gluten 100%, but if you are sensitive then you maybe able to have small exposures occasionally and manage the symptoms
The Vibrant Wellness Wheat Zoomer test offers a superior method for detecting both conditions, providing comprehensive insights that conventional blood tests may miss.
By adopting a gluten-free diet and supporting gut health through dietary and lifestyle changes, you can manage symptoms and improve your overall quality of life.
Related Post
Food Intolerances and Sensitivities
What are Food Intolerances and Sensitivities?
Food intolerances and sensitivities occur when the body has difficulty digesting certain foods or when a particular food triggers an adverse reaction in the digestive system.
Unlike food allergies, which involve an immediate immune response, food intolerances and sensitivities often result in delayed symptoms that can be challenging to identify and manage.
Common Symptoms of Food Intolerances and Sensitivities
Symptoms of food intolerances and sensitivities can vary widely and often overlap with other digestive issues. Common symptoms include:
- Digestive Problems: Bloating, gas, diarrhea, constipation, and abdominal pain.
- Headaches: Frequent headaches or migraines.
- Fatigue: Persistent tiredness and lack of energy.
- Skin Issues: Rashes, eczema, or acne.
- Joint Pain: Unexplained joint aches and pains.
- Mood Changes: Irritability, anxiety, and mood swings.
Causes of Food Intolerances and Sensitivities
Several factors can contribute to the development of food intolerances and sensitivities, including:
- Enzyme Deficiencies: Lack of specific digestive enzymes needed to break down certain foods (e.g., lactase deficiency leading to lactose intolerance).
- Dysbiosis: Imbalances in the gut microbiome can impair digestion and lead to sensitivities.
- Leaky Gut: Increased intestinal permeability allows partially digested food particles to enter the bloodstream, triggering immune reactions.
- Chronic Stress: Persistent stress can affect digestion and increase sensitivity to certain foods.
Diagnosing Food Intolerances and Sensitivities
Elimination Diet
How It Works
An elimination diet involves removing suspected trigger foods from the diet for a period (usually 4-6 weeks) and then gradually reintroducing them one at a time to observe any reactions.
Effectiveness
This method is highly effective in identifying specific food intolerances and sensitivities, as it directly correlates symptoms with dietary changes.
Challenges
Requires strict adherence and careful monitoring, which can be difficult for some people.
Advanced Stool Testing
- Identifying Dysbiosis: Comprehensive stool tests can reveal imbalances in the gut microbiome, infections, digestive enzymes and inflammation markers that may contribute to food sensitivities.
- Benefits: Provides a detailed analysis of gut health, which can inform targeted treatment plans to address underlying issues.
Vibrant Wellness Food Sensitivity Test
How It Works
This test measures the immune response to a wide range of foods by detecting specific antibodies (IgG and IgA) in the blood.
Advantages
Useful for individuals who cannot commit to an elimination diet or need quicker results. It provides a comprehensive overview of potential food sensitivities.
Limitations
While helpful, results should be interpreted alongside clinical symptoms and other diagnostic tools for a complete picture.
Managing Food Intolerances and Sensitivities
Management strategies typically involve dietary adjustments and addressing underlying gut health issues:
Dietary Changes
- Elimination and Reintroduction: Follow an elimination diet to identify and remove trigger foods.
- Personalized Nutrition: Develop a tailored eating plan that avoids identified triggers and includes nutrient-dense foods to support overall health.
- Hydration: Ensure adequate fluid intake to support digestion.
Supporting Gut Health
- Probiotics and Prebiotics: Support a healthy gut microbiome to improve digestion and reduce sensitivities.
- Digestive Enzymes: Supplementing with enzymes can aid in the digestion of problematic foods.
- Stress Management: Techniques like yoga, meditation, Nerva program and regular exercise can help manage stress and improve digestive health.
Oten food sensitivities don’t require total avoidance, and if you address the underlying cause then often you can reintroduce the food again.
Understanding and managing food triggers is important for maintaining optimal gut health and overall well-being.
While elimination diets are the gold standard for identifying specific triggers, advanced stool tests and the Vibrant Wellness Food Sensitivity Test offer valuable alternatives for those who need them.
By addressing underlying gut health issues and making informed dietary choices, you can effectively manage your symptoms and improve quality of life.
Related Post
The Low FODMAP Diet for IBS
What is the Low FODMAP Diet?
The low FODMAP diet is a dietary approach designed to reduce symptoms of digestive discomfort by limiting certain types of carbohydrates that are difficult to digest.
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols—types of short-chain carbohydrates that can be poorly absorbed in the small intestine.
This diet has been shown to be effective in managing symptoms of IBS, SIBO, dysbiosis, and other food sensitivities.
How Does the Low FODMAP Diet Work?
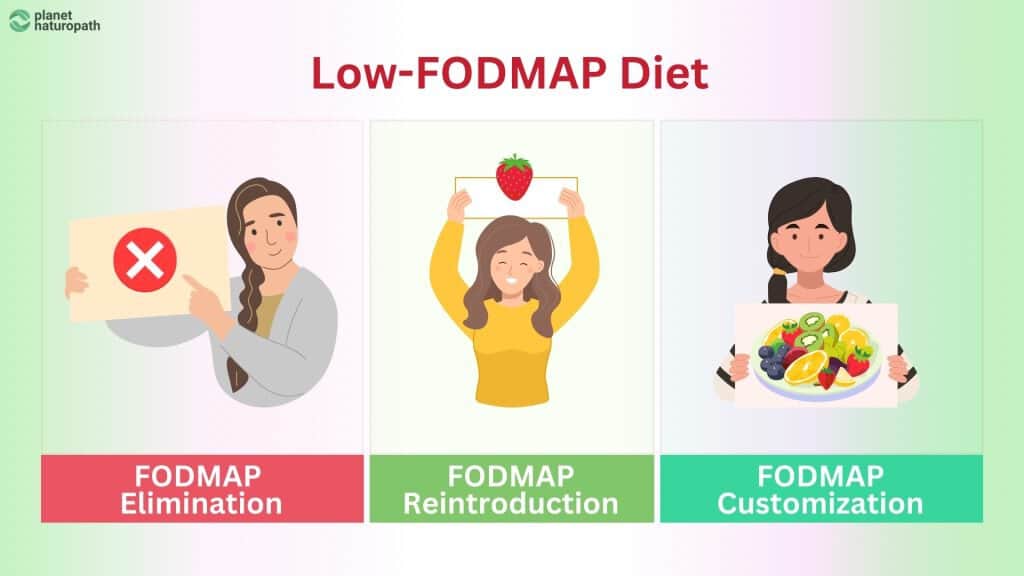
The low FODMAP diet involves three phases:
- Elimination Phase: All high FODMAP foods are removed from the diet for a period of 3-6 weeks to allow symptoms to improve.
- Reintroduction Phase: High FODMAP foods are gradually reintroduced one category at a time to identify which specific types cause symptoms.
- Personalization Phase: A long-term eating plan is developed that minimizes high FODMAP foods that trigger symptoms, however, for many people if they address the trigger they can eat these foods again.
Common High FODMAP Foods
High FODMAP foods include certain fruits, vegetables, dairy products, grains, and sweeteners. Examples are:
- Fruits: Apples, pears, and watermelon.
- Vegetables: Onions, garlic, and cauliflower.
- Dairy: Milk, yogurt, and soft cheeses.
- Grains: Wheat, rye, and barley.
- Sweeteners: High-fructose corn syrup and artificial sweeteners like sorbitol.
Benefits of the Low FODMAP Diet
Symptom Relief
Significantly reduces symptoms like bloating, gas, abdominal pain, and irregular bowel movements.
While many people are happy to get symptoms relief it is important to understand that this diet cuts out lots of super health foods and is not ideal for the long term health of the microbiome.
Identification of Triggers
Helps pinpoint specific FODMAPs that trigger symptoms, allowing for a more personalized diet.
Once the cause is addressed most people can tolerate more of these foods, this can take time and they may need to be slowly introduced.
Important Considerations
While the low FODMAP diet can be highly effective, it is important to emphasize that it should be a short-term solution.
Long-term adherence to a restrictive diet cannegatively impact the gut microbiome, and create unwanted stress around food choices. The goal should be to identify and address the underlying causes of digestive symptoms.
Addressing Underlying Causes
SIBO
Small Intestinal Bacterial Overgrowth can be a significant cause of FODMAP intolerance. Treating SIBO with antibiotics or herbal antimicrobials, alongside dietary changes, can improve symptoms.
Dysbiosis
Imbalances in the gut microbiome can lead to poor digestion of FODMAPs. Probiotics, prebiotics, and dietary changes can help restore balance.
Food Intolerances
Identifying and managing food intolerances through elimination diets and advanced testing can reduce reliance on a restrictive diet.
Advanced Testing
Advanced testing can provide valuable insights into the underlying causes of FODMAP intolerance:
- SIBO Breath Test: Identifies bacterial overgrowth in the small intestine.
- Advanced Stool Tests: Detects dysbiosis, infections, and inflammation in the gut.
- Food Sensitivity Tests: Identifies specific food intolerances that may contribute to symptoms.
The low FODMAP diet is an effective tool for managing gut symptoms, but it should be used as part of a broader strategy to address underlying causes.
By combining short-term dietary changes with advanced testing and targeted treatments, individuals can achieve long-term relief from digestive discomfort while maintaining a balanced and varied diet.
Related Post
Prebiotics and Probiotics For Optimal Gut Health
What are Prebiotics and Probiotics?
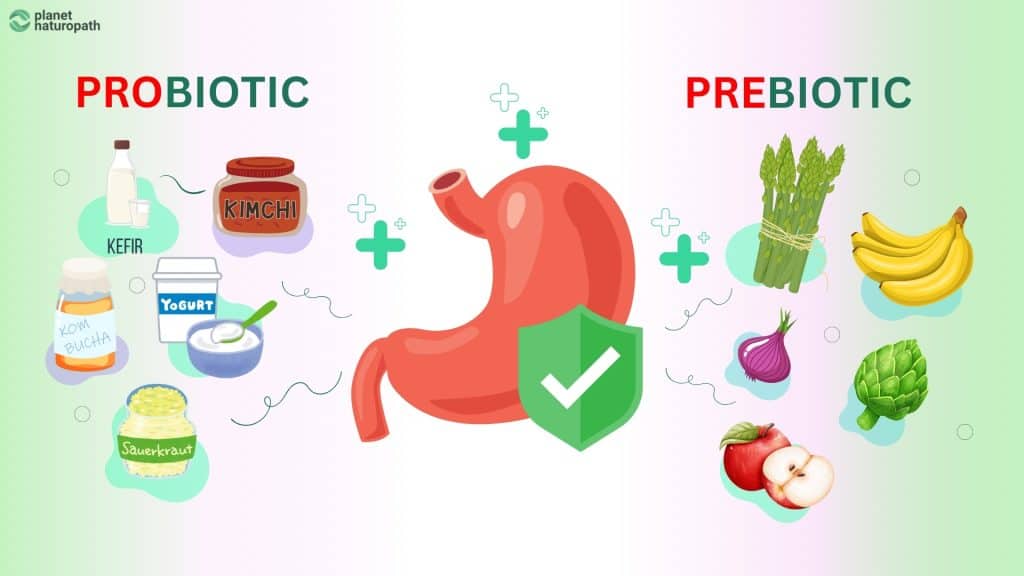
Prebiotics and probiotics are essential components of gut health, playing a significant role in maintaining a balanced gut microbiome.
Prebiotics are non-digestible fibers that serve as food for probiotics and other beneficial bacteria in the gut.
They help stimulate the growth and activity of these good bacteria, promoting a healthy gut environment.
These can be part of the diet and it is why are diverse diet is important for gut health, or they can be supplements if needed.
Probiotics are live beneficial bacteria that, when consumed in adequate amounts, confer health benefits to the host. They help replenish and maintain healthy gut flora, aid digestion, and support immune function.
It’s important to understand that all probiotics don’t have the same function so you need to take specific strains depending on your health goals.
Benefits of Prebiotics and Probiotics
Incorporating prebiotics and probiotics into your diet can offer numerous health benefits, including:
- Improved Digestion: Enhancing the breakdown and absorption of nutrients.
- Enhanced Immune Function: Supporting the body’s natural defense mechanisms.
- Reduced Inflammation: Alleviating symptoms of inflammatory conditions such as IBS and IBD.
- Balanced Gut Microbiome: Promoting a diverse and healthy population of gut bacteria.
Sources of Prebiotics and Probiotics
Dietary Sources
Probiotics
- Yogurt: Contains live cultures of beneficial bacteria. (not all yogurt contain therapeutic strains of bacteria)
- Kefir: A fermented milk drink rich in probiotics.
- Sauerkraut and Kimchi: Fermented vegetables that provide probiotics.
- Miso: A fermented soybean paste used in Japanese cuisine.
- Tempeh: A fermented soybean product that offers probiotics.
Prebiotics
- Garlic and Onions: Rich in inulin, a type of prebiotic fiber.
- Bananas: Contain fructooligosaccharides (FOS) that promote beneficial bacteria.
- Asparagus and Leeks: High in inulin and other prebiotic fibers.
- Whole Grains: Such as oats and barley, which contain prebiotic fibers.
- Legumes: Beans, lentils, and chickpeas are excellent sources of prebiotics.
Supplemental Sources
Probiotic Supplements
- Capsules and Tablets: Contain specific strains of beneficial bacteria, such as Lactobacillus, Bifidobacterium, Akkermansia and spore based probiotics.
- Probiotic Drinks: Beverages like kombucha and certain kefirs fortified with live cultures.
Prebiotic Supplements
- Powders and Capsules: Contain concentrated forms of prebiotic fibers like Sunfiber, inulin, FOS, and galactooligosaccharides (GOS).
Choosing the Right Prebiotics and Probiotics
Selecting the right prebiotics and probiotics involves considering individual health needs and specific gut health goals. Here are some tips:
- Diverse Strains: Choose probiotics with multiple strains of beneficial bacteria for broader gut health benefits.
- Prebiotic Types: Select prebiotics that are compatible with your digestive system to avoid discomfort.
- Quality Brands: Opt for reputable brands that ensure the viability and efficacy of their products through rigorous testing.
The Synergy of Prebiotics and Probiotics
The combination of prebiotics and probiotics, known as synbiotics, offers synergistic benefits for gut health.
Prebiotics provide the nourishment probiotics need to thrive, enhancing their effectiveness and promoting a balanced gut microbiome.
Including both in your diet or supplement regimen can optimize digestive health and overall well-being.
Prebiotics and probiotics are crucial for maintaining optimal gut health. By incorporating a variety of prebiotic and probiotic foods into your diet and considering quality supplements, you can support a balanced and healthy gut microbiome.
This, in turn, can improve digestion, boost immune function, and reduce inflammation, contributing to overall health and vitality.
[Related post] Probiotics versus Prebiotics: Which is Best for Your Health?
Related Post